Demographics of New Orleans and early COVID-19 Hot Spots in the U.S.
First Published: Mar 25, 2020
Analysis Updated: Apr 20, 2020
This webpage highlights key demographic data relevant to mitigating the spread of COVID-19 and related economic impacts in New Orleans. Indicators include age distribution, poverty levels, access to vehicles and the internet, along with comparisons to Seattle, Westchester County, NY, and New York City. This webpage is intended to inform decisionmakers in policymaking, program design, and resource allocation.
Income and poverty
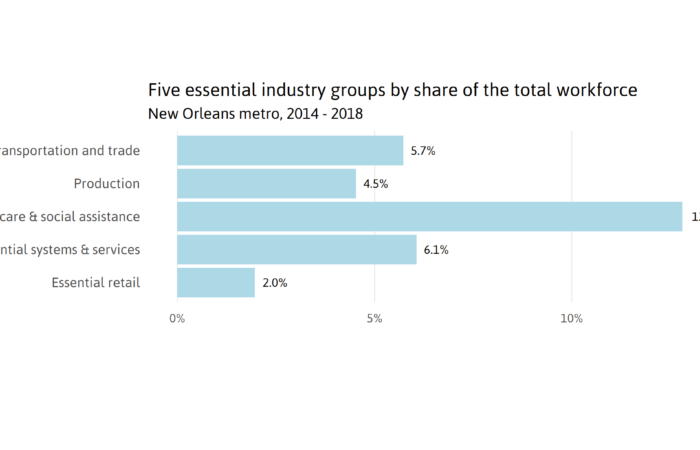
Income and poverty measures can indicate the extent to which a community may be able to successfully adhere to COVID-19 mitigation measures (such as “stay at home” and “quarantine family members who are sick”). Lower-income individuals are more likely to be living in crowded households where there are more people than rooms, making quarantining sick family members more difficult. i Low-income individuals are more likely to be working in service positions on the front line of COVID-19 including as at-home health aides for seniors, grocery store clerks, and nannies, and may not be able to “stay at home.” ii Lower-income individuals are more likely to experience health conditions such as high blood pressure iii and diabetes iv that may increase the likelihood of hospitalization and death among COVID-19 patients. v There are a myriad of reasons why lower-income and poorer communities will be more vulnerable to the COVID-19 virus as explored in additional indicators on this webpage.


Households with zero net worth
Savings or wealth is very important for supporting a family’s ability to be resilient in the face of health and economic shocks. Liquid asset poverty rates indicate the percent of households that do not have enough liquid net worth (savings) to survive at the poverty level for three months without income. When a large share of a community does not have sufficient savings, it can have severe implications for residents who have been laid off due to COVID-19-related business closures and residents who bear unexpected health costs due to contracting COVID-19.


Access to vehicles
The share of households without access to a vehicle can help cities determine the best approach for making available widespread COVID-19 testing. Drive-up testing will be less effective in cities and counties where larger shares of the population do not have access to vehicles. Additional means of testing should be considered for most cities and counties.

Internet access
Internet access is an important indicator of access to information, ability to work from home, and ability to participate in online learning. An increasingly common way to access the Internet is through a smartphone or some other cellular device. But having access only through a smartphone restricts ability to fully leverage the Internet to complete at-home work tasks such as writing documents, assisting children with homework, creating content for an internet business, or analyzing data about your neighborhood. Access only at locations inaccessible during lockdown refers to households who only have access through group locations such as school, work, a library, or coffee shop—all of which are not available given “stay at home” orders.

Housing costs relative to incomes
This indicator measures the share of renters paying more than half of their household income on rent. When the majority of a paycheck goes toward rent, families often have to make difficult choices between food, medicines, and utilities. When incomes are lost, families that are severely “housing cost burdened” may suddenly face homelessness. vi The COVID-19 crisis and related layoffs of low-wage service workers could significantly increase housing instability in cities where many renters are already severely housing cost burdened (paying more than 50 percent of their pre-tax household income on rent and utilities).

Underlying health conditions (comorbidities) related to COVID-19
Emerging studies have identified high blood pressure, diabetes (or “sugar diabetes” as it is called by many New Orleanians), coronary heart disease, chronic obstructive pulmonary disease (COPD—often associated with smoking), chronic kidney disease, and cancer as pre-existing health conditions that may increase the likelihood of severe outcomes for people who get infected with COVID-19. vii Cities with higher rates of these health conditions may see higher hospitalization rates and more deaths from COVID-19 infections.

Age distribution
Early studies on the COVID-19 virus indicate that the virus more seriously affects older adults as well as those with pre-existing health problems. Death rates have been highest among older adults. viii Nonetheless, these studies also reveal that more adults age 20 to 64 have been hospitalized with COVID-19 disease than adults age 65+ in the United States. ix The age distribution of a community can help inform likely COVID-19 hospitalization and death rates.

Living wage and annual household costs in New Orleans
According to MIT, the cost to live in New Orleans without any subsidies in 2018 for one adult with one child was $23.93 per hour or $49,778 annually. For households of one adult and one child, annual costs are: fair market rent and utilities for a two bedroom apartment at $12,033, food at $6,877 based on the USDA low-cost food plan, gas and routine maintenance of a car at $10,689, and employer-sponsored health insurance, medical services, drugs and medical supplies at $8,003.

Notes:
- Housing: HUD Fair Market Rents
- USDA low-cost food plan
- Transportation: Transportation costs cover operational expenses such as fuel and routine maintenance as well as vehicle financing and vehicle insurance but do not include the costs of purchasing a new automobile. These costs were further adjusted for regional 1
- Medical: (1) health insurance costs for employer sponsored plans, (3) medical services, (3) drugs, and (4) medical supplies
- Other: clothing, personal care items, and housekeeping supplies.
- Taxes: federal and state income taxes
- Child care: state-level estimates published by the National Association of Child Care Resource and Referral Agencies in 2015.
- Families with one child are assumed to have a ‘young child’ (4 years old). Families with two children are assumed to have a ‘young child’ and a ‘child’ (9 years old).
Race/Ethnicity in New Orleans
Understanding the racial make-up of the city of New Orleans is essential for clarity about who is likely most affected by the twin health and economic crisis that COVID-19 represents. Nearly 60 percent of New Orleanians are African American, 31 percent are white, 5.6 percent are Hispanic, and 2.9 percent are Asian.

Income and poverty by Race/Ethnicity in New Orleans
African Americans, who make up a majority of New Orleans, earn significantly less than white New Orleanians. According to the most recent data (from 2018), African American households earned about 1/3 of what white households earned on average. The median household income for black households in New Orleans was $24,813, compared to $69,852 for white households, $55,616 for Asian households, and $38,487 for Hispanic households. In other words, half of all black families in New Orleans earned less than $25,000 in 2018.

Fully 32 percent of all black households in New Orleans live in poverty, compared to only 10 percent of white households. Lower-income individuals are more likely to be living in households where there are more people than rooms, making quarantining sick family members more difficult. Emerging research suggests that the virus is more likely to be spread among household members or individuals traveling together, than other contacts. x

Households with zero net worth by Race/Ethnicity in New Orleans
Savings or wealth is very important to a family’s ability to be resilient in the face of health and economic shocks. When a large share of a community does not have sufficient savings, it can have severe implications for residents who have been laid off due to COVID-19-related business closures. vi Families without income often have to make difficult tradeoffs among basic necessities such as groceries and medicines. xi Liquid asset poverty rates are the percent of households that do not have enough savings to survive at the poverty level for three months without income.
In New Orleans, while 54 percent of all households are in “liquid asset poverty,” this measure broken down by race shows that 71 percent of black households are in “liquid asset poverty” compared to 29 percent of white households and 59 percent of Hispanic households. Similarly, 33 percent of black households in New Orleans have zero net worth compared to 16 percent of white households, and 27 percent of Hispanic households.


Households with individuals over 60 living with grandchildren
Grandparents are being advised to isolate themselves from grandchildren 1 . But when grandparents live with their grandchildren, their exposure to COVID may be increased. In New Orleans, 12.2 percent of all black people 60 years and older live in multigenerational households while only 3.8 percent of white elders do.

Footnotes
1 U.S. Centers for Disease Control. (2019) Caring for Children https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/children.html
Sources
i Lopoo, L. and London, A. (2018). How Does Household Crowding Affect Education Outcomes? Retrieved from https://housingmatters.urban.org/research-summary/how-does-household-crowding-affect-education-outcomes
ii Ross, M. (2020) A Closer Look at Low-wage Workers Across the Country. Brookings Institution. Retrieved from https://www.brookings.edu/interactives/low-wage-workforce/
iii Carroll, W. (2011). Hypertension in America: Estimates for the U.S. Civilian Noninstitutionalized Population, Age 18 and Older, 2008. Medical Expenditure Panel Survey. Retrieved from https://meps.ahrq.gov/data_files/publications/st315/stat315.pdf
iv Gaskin, D. et al. (2014) Disparities in Diabetes: The Nexus of Race, Poverty, and Place. American Journal of Public Health. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4021012/
v Guan, W. J., Liang, W. H., Zhao, Y., Liang, H. R., Chen, Z. S., Li, Y. M., … and Ou, C. Q. (2020). Comorbidity and its impact on 1,590 patients with COVID-19 in China: A Nationwide Analysis. medRxiv. Yang, J., Zheng, Y., Gou, X., Pu, K., Chen, Z., Guo, Q., … & Zhou, Y. (2020). Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. International Journal of Infectious Diseases.
vi Severe housing cost burden: Percentage of households that spend 50% or more of their household income on housing.(2020). County Health Rankings and Roadmaps, a Robert Wood Johnson Foundation program. Retrieved from: https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model/health-factors/physical-environment/housing-transit/severe-housing-cost-burden
vii Guan, W. J., Liang, W. H., Zhao, Y., Liang, H. R., Chen, Z. S., Li, Y. M., … and Ou, C. Q. (2020). Comorbidity and its impact on 1,590 patients with COVID-19 in China: A Nationwide Analysis. medR
viii The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. (2020) The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020. Retrieved from https://github.com/cmrivers/ncov/blob/master/COVID-19.pdf
ix CDC COVID-19 Response Team. (2020) Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020. Retrieved from https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm?s_cid=mm6912e2_w#F2_down
x Bi, Q. et al. (2020) Epidemiology and Transmission of COVID-19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. Retrieved from https://www.medrxiv.org/content/10.1101/2020.03.03.20028423v3
xi CDC COVID-19 Response Team. (2020) Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020. Retrieved from https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm?s_cid=mm6912e2_w#F2_down